September is Childhood Cancer Awareness Month. The following article is meant to raise awareness of von Hippel-Lindau disease (VHL) and to help the public learn about state-of-the-art VHL care available in San Antonio. The Mays Cancer Center is recognized as a VHL Clinical Care Center by the VHL Alliance.
Brianna Garcia wondered why her heart raced when she exercised and why she was tired all the time. Her gynecologist in Laredo noticed abnormal periods, high blood pressure and elevated blood sugar in the 15-year-old.
What could be causing these symptoms?
In April Brianna’s doctor referred her to a team of specialists at The University of Texas Health Science Center at San Antonio, a 2½-hour drive away. Six weeks of care followed at University Hospital, a University Health facility, where health science center experts in multiple disciplines unraveled Brianna’s medical mystery.
Because Brianna’s mother, Dora Alicia Olvera Garcia, had died of metastatic pancreatic cancer, faculty pediatric oncologists and radiologists conducted imaging studies to look for tumors.
The pediatrics inpatient team worked up the youngster’s high blood pressure, and the pediatric endocrinology team evaluated factors involved in the high blood sugar.
Answers came swiftly.
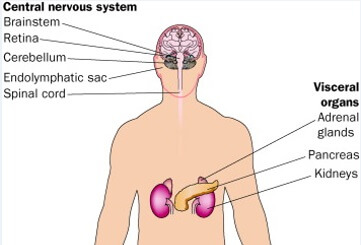
Ultrasound images of the kidneys showed a mass on the adrenal gland above one kidney. The adrenal glands, one on top of each kidney, secrete hormones that regulate metabolism, stress response and blood pressure, among other functions.
“This tumor, called a pheochromocytoma, played a significant role in the high blood pressure, rapid heart rate and elevated blood sugars,” said Maria “Sukie” Rayas, MD, assistant professor of pediatric endocrinology in the health science center’s Joe R. and Teresa Lozano Long School of Medicine.
Imaging next revealed a pair of lesions in Brianna’s liver and a mass on her left ovary. Hematology-oncology specialists again were consulted. Further imaging found multiple small masses in the pancreas.
Seeking a genetic basis
A genetic evaluation was happening simultaneously. Texts and calls now flowed between various members of the group, including Gail Tomlinson, MD, PhD, professor of pediatric hematology/oncology, who works with the Greehey Children’s Cancer Research Institute and with the Mays Cancer Center Genetic High-Risk Cancer Screening team on Brianna’s case. Patricia Dahia, MD, PhD, an internationally known expert on pheochromocytoma and other cancers known as neuroendocrine tumors, provided extra knowledge about these types of tumors. Dr. Dahia is a professor of medicine and member of the Mays Cancer Center, home to UT Health San Antonio MD Anderson Cancer Center. Dr. Tomlinson occupies the Greehey Distinguished Chair in Cancer and Genetics at the health science center.
The genetic study rendered a verdict: von Hippel-Lindau (VHL) disease, an inherited disorder marked by formation of benign and malignant tumors potentially anywhere in the body.
Several nuclear medicine scans and full-body evaluations further characterized Brianna’s tumors. The liver lesions were biopsied and found to be benign. On May 10, an advanced endoscopy biopsy of the pancreatic masses was performed by Sandeep Patel, DO, associate professor of medicine and pediatrics, medical director of University Hospital endoscopy. The pancreatic masses were neuroendocrine tumors. The adrenal and ovarian masses also needed to be addressed.

Strategy and surgery
Brianna’s case was discussed at an hourlong pediatric tumor board, a think tank of specialists from the Mays Cancer Center and departments of the Long School of Medicine. The group began planning additional treatments, including surgery.
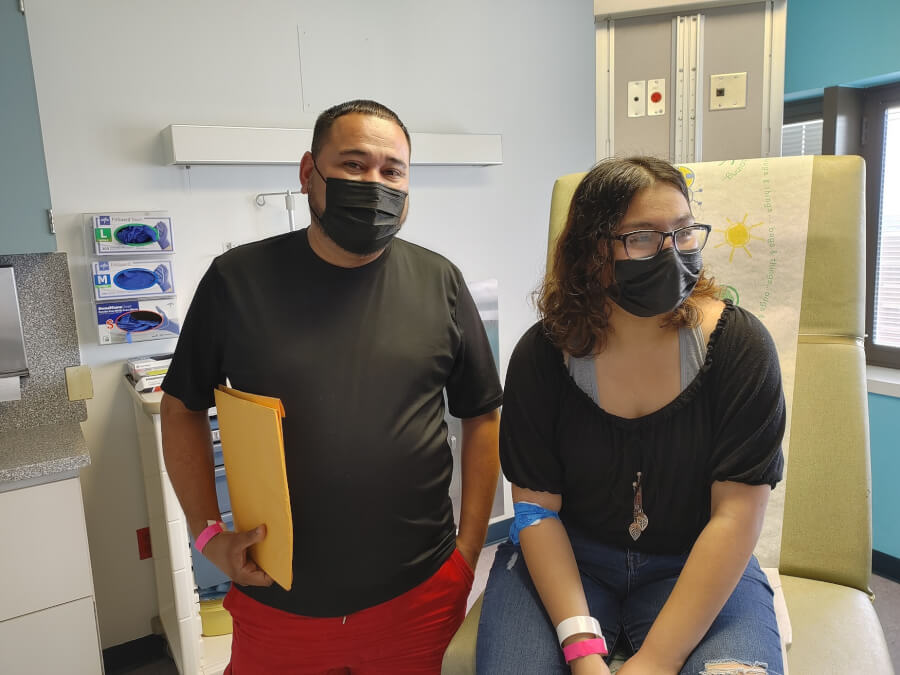
Family meetings were held with Brianna and her father, Julio Garcia. The pheochromocytoma was secreting normetanephrine, a substance that “gets the body completely revved up,” said Aaron Sugalski, DO, associate professor of hematology-oncology in the Long School of Medicine and medical director of the University Hospital Pediatric Blood and Cancer Center. Brianna was receiving insulin and blood pressure medications.
More planning meetings ensued. Danielle Fritze, MD, of the UT Health San Antonio Transplant Center, and Barry Cofer, MD, of the pediatric surgery faculty and San Antonio Pediatric Surgery Associates, planned a complex surgery to remove the adrenal mass. This took place on May 26. Two days later, Edward Kost, MD, professor of obstetrics and gynecology, removed the benign left ovarian mass. The team will continue to monitor the pancreatic masses and the benign liver lesions.
“Every step of the way, we’ve considered what would optimally stabilize Brianna’s condition and improve her long-term outlook in the best way possible,” Dr. Fritze said. “Brianna is an extremely strong and positive person, and our team will be right there to support her as she moves forward with VHL.”
Brianna’s blood pressure and sugars normalized after surgery. She recovered well from the surgeries with no complications and returned home to Laredo on June 2. Dr. Sugalski saw her for follow-ups in June and July. Results of a blood and urine study in June were normal. Importantly for the long term, she had no immediate need for chemotherapy or radiation, said Dr. Sugalski, who will be guiding her follow-up care. “I feel confident that we did everything that was right for her,” he said.
Mom’s struggle
Brianna’s mother, Dora, probably had VHL, which increased the children’s chances of inheriting the disorder. Brianna and her big sister, Kimberly, 17, grew up watching their mother battle cancer. Dora died too young, at the age of 38 in 2015. Their father, Julio, was depressed and confused. Brianna was only 9 and Kimberly 11. “He didn’t want us to go through so much without our mom,” Kimberly said.
Genetic tests have confirmed that Kimberly has VHL, too. She accompanied Brianna and Julio to the hospital July 16 to meet with Dr. Sugalski and Dr. Tomlinson and prepare for her own testing. Imaging revealed that she has a left ovarian mass; it is currently being evaluated.
“Now that they found it [VHL], they can be treating us,” Kimberly said.
Experienced team
Julio said he is comforted by the fact that multiple specialists are monitoring Brianna and Kimberly. One of Laredo’s more famous native sons, Francisco G. Cigarroa, MD, professor and surgeon at UT Health Science Center San Antonio and the institution’s former president, visited them when Brianna was in the hospital.
Reflecting this breadth of expertise, the Mays Cancer Center recently was named a VHL Alliance-recognized Clinical Care Center for unique capability and experience in treating the disorder. This level of care simply can’t be found in many places. Chethan Ramamurthy, MD, assistant professor of medical oncology, and Deepak Pruthi, MD, MS, assistant professor of urologic oncology, are the VHL center directors. The center provides comprehensive genetic testing and counseling, screening, targeted therapies and surgical expertise to care for patients with von Hippel-Lindau disease.
Family life
Kimberly is a senior and Brianna a sophomore this fall at Laredo Martin High School. They are one year and eight months apart in age. “We fight about different stuff. I think that’s how we show our affection, by fighting,” Kimberly said with a smile.
Over the summer, they stayed awake until 6 a.m. before going to sleep, she said. Typical teenagers. Now, back in school, Kimberly doesn’t know yet what she wants to do next, but she may go to college and prefers to stay close to home.
Brianna likes to draw. “Realism,” she said. She drew portraits of her mom and some of her friends and posted them online, drawing a ton of likes.
Their mother’s gravestone is in Nuevo Laredo, about 15 minutes from their house. It is in the Panteon Municipal Numero Dos cemetery. They go there a couple of times a month and plant flowers.
Talking about her, words come at a premium now, standing there in a clinic room at University Hospital.
“Strength comes from our family,” Julio said. In the years since Dora’s passing, he married Erica de Alva, and they are raising a blended family with seven children. He works at a warehouse as a truck driver and is a hard worker.
Do they like the beach? “Yeah, we go a lot. South Padre,” Kimberly said.
Staying alert to stay safe
Dr. Gail Tomlinson entered the clinic room along with two genetic counselors, Rachel Wyatt and Emily Berenson. Ms. Wyatt explained that there are two copies of each gene in cells. The copies are called alleles. One allele is inherited from the father and one from the mother.

In the girls’ case, she said, there is a tiny misspelling on one of the copies of the VHL gene, which normally suppresses tumor formation.
Without that brake in place, tests are regularly needed to detect changes before they become large problems. “Sometimes with VHL, very tiny nodules develop inside the eye and grow very slowly, so you might not notice them,” Dr. Tomlinson said, citing vision as an example. “It is important to recognize them sooner rather than later, so we recommend a very thorough eye exam.”
The nodules are little collections of blood vessels that grow to form small lumps. “Sometimes they start inside your brain, and it’s not cancer, but it’s a little lesion,” Dr. Tomlinson said, citing another example. “It can start out small and get bigger, so we do an MRI of the brain regularly to make sure there is nothing significant.”
Periodically the girls will also have an ultrasound of the abdomen. They will be seen in clinic every six months to a year, and it may be possible to do some of the imaging studies in Laredo, Dr. Tomlinson said.
Encouragingly, she said most of the problems that occur in VHL can be treated. The key is to stay on top of it and catch the nodules early.
“So that’s what we mean by keeping you healthy,” Dr. Tomlinson said to the girls. “We just want to be on the lookout, and if there are any VHL-associated growths or lesions inside your body, we want to know about them early.”
The misspelled gene usually comes from the parents, and Brianna and Kimberly are advised of the risk of passing it on to children they may have. “Now that we have two siblings that have the same condition, it suggests that your dad or your mom passed on the misspelled gene,” Ms. Wyatt said. She then added:
“It is really important with genetics to know that we can’t control the genes we pass on, so whether it was inherited or not, it wasn’t something you guys ate or drank, or did or did not do, that caused this.”
“It was no one’s fault, no one could control having it,” Dr. Tomlinson added. “But now we know, so we can try to control what happens in the future by just trying to keep everybody safe.”
In addition to helping the two teens face their cancer risks, the genetics team offered to work with extended family members including an older brother. The team provides outreach services to The University of Texas Education and Research Center at Laredo through telehealth. The team established a comprehensive genetic counseling service to sites throughout South Texas including Laredo through a previous grant from the Cancer Prevention and Research Institute of Texas.

‘The best team behind them’
The girls said their father is a prankster. “Like when he gets the salt, he opens the bigger lid, so you put a lot of salt,” Kimberly said. He especially does it to their four stepbrothers, she said, with a gleam in her eye.
It’s unlikely that the medical team can save Brianna and Kimberly from these pranks, and what the future holds is uncertain. But this is bedrock: the team has the knowledge, the talent and the experience to help them stay healthy.
“Caring for Brianna has given all of us a great deal of pride in the passion, commitment and compassion we have for every patient, and the way in which we are able to come together as an interdisciplinary team is inspiring,” Dr. Cigarroa said. “This is what being a physician truly means.
“Hopefully research in this area can also help us in understanding von Hippel-Lindau disease,” Dr. Cigarroa said. “Our patients have a long road ahead of them, but they have the best team behind them.”
For more information about VHL diagnosis and treatment, contact Mays Cancer Center family services at (210) 450-5570.


